What would you write in your report?
I am grateful to Kate Hardy from Freeman Hospital, Newcastle upon Tyne, for providing this ECG.
Dr Dave Richley
Answer Added 26.11.24
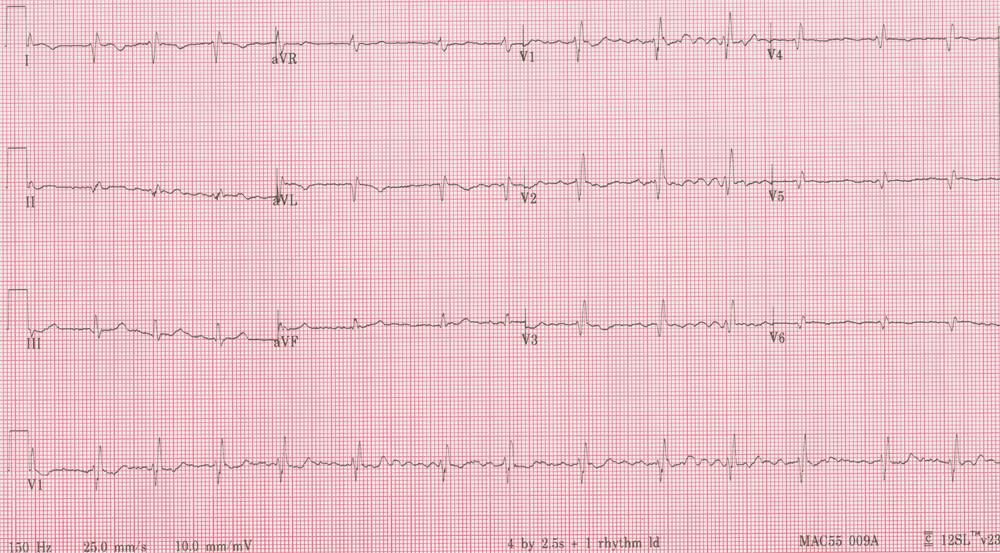
The rhythm is atrial fibrillation (AF) and there is a right axis deviation. There is also right bundle branch block (RBBB) and unusually, as Arron Pearce pointed out, the second R wave is taller in V2 than in V1. Why could this be? Additionally, the chest leads show diminishing QRS amplitudes from V2 to V6.
This is a case of mirror-image dextrocardia but it’s more difficult to recognise than usual because of the AF: there are no P waves and abnormal P wave polarity is usually one of the most important clues to the presence of dextrocardia. Right axis deviation is a feature of dextrocardia but as contributors to the discussion have said, there are several possible causes of right axis deviation and it is the combination of the abnormal appearances here that should raise the suspicion of dextrocardia.
Normally, of course, in dextrocardia the chest lead complexes not only diminish in size towards V6, they remain predominantly negative in all the chest leads because the ventricular depolarisation vector is directed to the right. This is not quite what we see here because although the QRS complexes get progressively smaller towards V6, they are never mostly negative in polarity. This is because of the RBBB. In RBBB there is delayed and prolonged depolarisation of the right ventricle, which normally causes a terminal, broad S wave in V5 and V6. Here because the morphological right ventricle is on the left, the terminal QRS forces are directed leftwards, producing a terminal R wave in V5 and V6 (and I, II and aVL).
If I were reporting on this ECG I think I would recommend that the recording be repeated with right-sided chest leads. Such a recording was in fact done and it is shown in figure 2, where the chest leads run from V2 (or V1R) to a right-sided V6 (V6R). The almost-normal QRS amplitudes in the modified chest leads confirm the suspicion of dextrocardia. However, there is a failure of the initial R wave to progress normally in amplitude from V1R-V3R, and a more fragmented QRS in V3R and V4R than would normally be attributed to RBBB alone, and this may be evidence of old anterior myocardial infarction.
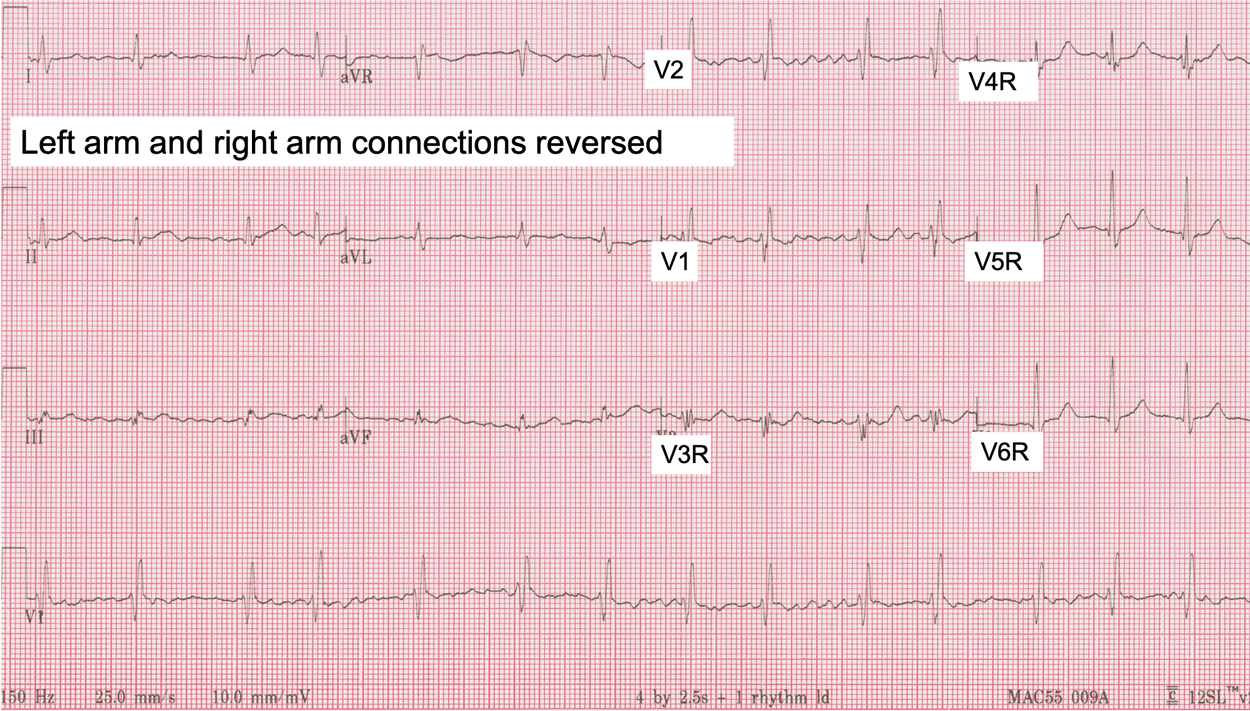
Many people like the ECG in dextrocardia to be recorded with reversed right arm and left arm connections to ‘normalise’ the limb lead appearances. I’m not sure that this is necessarily particularly helpful, but for completeness figure 2 shows the ECG with left arm and right arm connections reversed as well as right-sided chest leads.
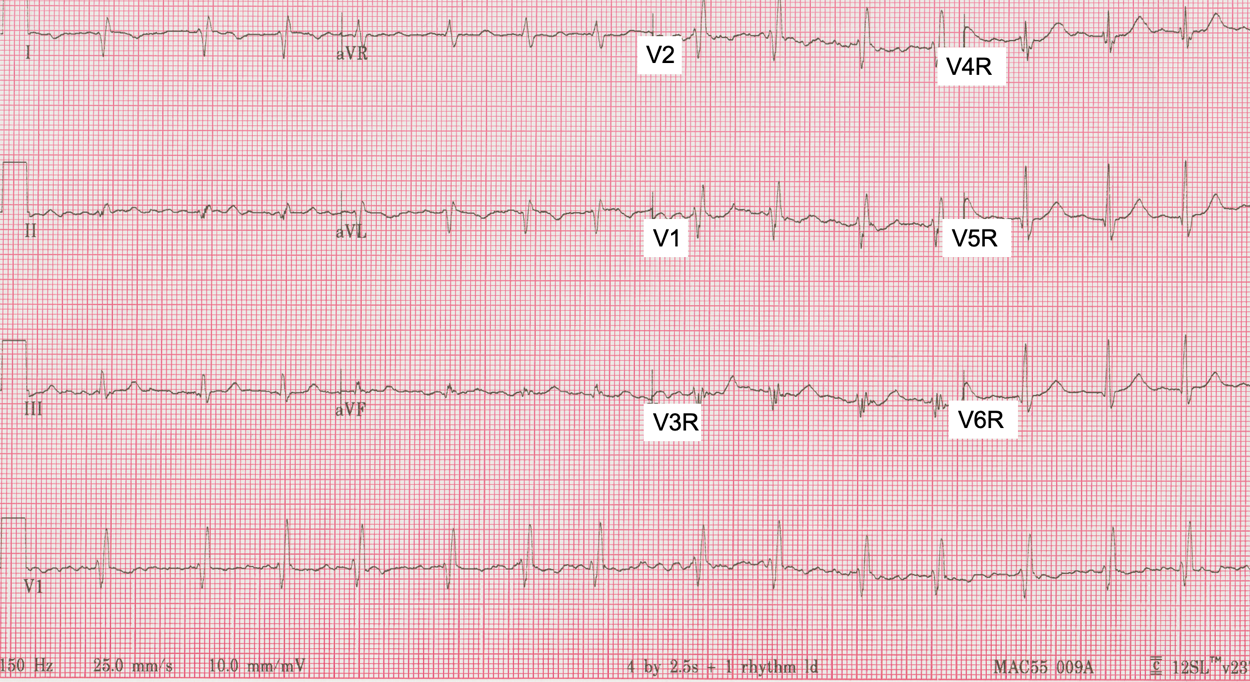
Figure 1: ECG recorded with right-sided chest leads.

Initial thoughts were
Af
Transposed R and L arm leads
Partial RB3
Low voltage precordial leads – suggestive of maybe pneumothorax or effusion or maybe she had previous lung resection?
Thanks for kicking off the discussion, Mags. I won’t reply in detail yet, but are there any other possible explanations for the findings?
Well she could have dextrocardia but I’d have thought that might have been exposed before she reached 70yrs
Atrial fibrillation. Right axis and some T wave inversion anterior lat leads. ?PE.
Thanks, Esther. I agree with AF and right axis deviation but are there any other possible explanations for what we see?
? COPD, Mitral stenosis with Pulmonary hypertension
Right axis deviation
Low voltage QRS complexes,V4-V6
Probable LAE which lead to the Af
I’d opt for the Mitral Stenosis as Im guessing she would have been diagnosed with COPD earlier
Interesting suggestions – thanks, Wayne. I’ll refrain from commenting further for the time being.
Atrial fibrillation with ventricular response of 78bpm, RAD and RBBB.
Low voltage.
Another scenario is this patient is a dextrocardia patient but highly unlikely for that age.
Interesting analysis, Ramadan. I wouldn’t rule out dextrocardia on the basis of age because we just don’t have a detailed enough history.
Abnormal Q waves in the anterior and lateral leads post MI?
Thanks, Sonia. Would MI explain everything here?
LA-RA lead reversal AF, precordial hypovoltage
Thanks, Fermi. Are there any other possible explanations that could account for what we see?
Interesting case, as always.
Atrial fibrillation with a modest ventricular response (HR 84).
Obvious from V1-3 that this is RBBB. Given this, one would expect typical “RBBB changes” in the lateral chest leads, which we don’t see, suggesting either a structural problem, inferior displacement of these leads (to avoid breast tissue maybe), or increased insulation between the electrodes on the chest wall and the heart (like from a pneumothorax or pleural effusion or ??).
In the limb leads, we also do not see the typical wide/slurred S waves in I and aVL and there is an apparent RAD — this is explained by RA/LA switch.
With lead errors corrected, we’re left with what should be a simple RBBB pattern, although I’m not 100% sure why V4-6 look diminutive and unlike RBBB.
A few differentials come to mind, including the entities mentioned earlier (to explain V4-6):
1. As the HR alone does not explain her presentation, and being unable to physically see/examine this patient, ?Mitral stenosis as a cause of AFib and breathlessness. Any combination of valvular pathology could also explain the presentation
2. ?Acute PE — evidence for this is not strongly suggested by what we see alone
3. ? Cardiac amyloidosis — this could explain the arrhythmia, conduction abnormality, and unusual QRS complexes we see, barring lead misplacements
I’m sure there are other possibilities. I’ll wait for the reveal.
Thanks, Onyinye – some good thoughts there, but I wonder if there is possibility you have missed.
Haha. Yes.
If it is dextrocardia, the RBBB pattern has thrown me off what I would normally expect to see in V4-6.
AFib also throws off as I cannot appreciate P wave axis.
1.dextrocardia
2.af
3.CRBBB
Very succinct, wangchangkun, and maybe you’ve cracked it!
I think we can all agree that this is AF with RBBB, however, there are several possibilities to consider when assessing the rest of the morphological abnormalities. This a list of possibilities, starting from most to least likely, in my opinion:
1 – Dextrocardia – there poor primary r wave progression with diminishing voltage through the precordial leads. In addition, V2 has the largest secondary R wave – in most of my examples of RBBB, the tallest secondary R waves are seen in V1
2 – Normal heart position (situs solitus) with left arm ↔ right arm lead reversal with old anterolateral infarction – AF does make it difficult to be certain in cases where lead reversals are suspected due to lack of P waves
3 – Dextrocardia with only mirrored chest electrodes to account for this (+ old anterolateral infarction) – this approach is mentioned in the SCST guidelines (large R’ V2 makes this less likely, unless V1/V2 switched or misplaced)
4 – Normal heart position with both the limb leads and the chest leads mirrored (exceptionally rare, however, I have seen this before, the person did not know what they were doing!)
In a breathlessness patient with AF and RBBB, we should consider pulmonary embolism. That being said, I think that she had dextrocardia which can cause breathless or perhaps the AF is new and causing the symptoms (controlled rate may suggest AV nodal/beta blockers or a slight degree AV node disease).
Immaculately argued, as always, Arron. Thanks.
Provisional report only: Atrial fibrillation with a moderate ventricular response resolving an effective ventricular rate of 85bpm in a setting of Dextrocardia with a Right Bundle Branch Block.
For clairifyed report please, if possible, repeat the ECG under the following two conditions:
Repeat the ECG using standard lead placement taking particular care to ensure correct lead placement, AND
Repeat the ECG using the following alternate lead placement pattern: swap the RA lead with LA lead. Swap the RL lead with the LL lead Set up the precordial leads in V1R-V6R ( right precordial) pattern.
Resubmit both ECGs for analysis.
RATIONALE:
A. In all leads atrial signals appear to be either absent or disorganised and inconsistent. The ventricular rhythm is irregularly irregular. These things suggest AF.
B. Overall the voltage is low but particularly in the left precordial leads where the voltage < 6mm in each lead and progressively diminishes out to V6. There is incomplete transition and marked right axis deviation (+120). There are apparent Q waves in I II aVL and throughout the precordium. These factors are consistent with standard leads looking at a mirrored image of the heart, i.e. ’Situs Invertus’ Dextrocardia
C. There is an rSR’ pattern in V1(V2R) and V2 (V1R) with a QRS interval of ~ 120msec. aVr is isoelectric and has a slightly widened ‘looped’ terminal S wave. This is an expected pattern for a high lateral lead with a RBBB. Thus it is consistent seeing it in this setting where aVr is equivalent to aVL. These observations suggest a RBBB in a patient with Dextrocardia.
D. Thing to clarify with the repeat ECGs:
The repeat standard ECG should show the exact same result as presented here and should therefor help rule out lead misplacement;
The alternate ECG should:
confirm AF with a moderate ventricular response and
should appear with a normal frontal axis and a normal precordial R wave progression.
aVL and aVR should be reversed when compared to the standard lead placement and
the pattern in the right precordial and high lateral leads should confirm or refute the RBBB.
make sure also in the alternate lead placement ECG that the voltage is now back within normal limits
Highight any other abnormality masked by the anomalous heart view
Thanks, Jeff – a very comprehensive analysis.